Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).[10] It was first identified in December 2019 in Wuhan, China, and has since spread globally, resulting in an ongoing pandemic.[11][12] As of 27 May 2020, more than 5.59 million cases have been reported across 188 countries and territories, resulting in more than 350,000 deaths. More than 2.28 million people have recovered.[9]
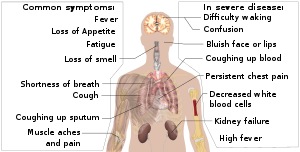
Common symptoms include fever, cough, fatigue, shortness of breath, and loss of smell and taste.[6][7][13] While the majority of cases result in mild symptoms, some progress to acute respiratory distress syndrome (ARDS) likely precipitated by a cytokine storm,[14] multi-organ failure, septic shock, and blood clots.[15][16][17] The time from exposure to onset of symptoms is typically around five days but may range from two to fourteen days.[6][18]
The virus is primarily spread between people during close contact,[a] most often via small droplets produced by coughing,[b] sneezing, and talking.[7][19][21] The droplets usually fall to the ground or onto surfaces rather than travelling through air over long distances.[7] Less commonly, people may become infected by touching a contaminated surface and then touching their face.[7][19] It is most contagious during the first three days after the onset of symptoms, although spread is possible before symptoms appear, and from people who do not show symptoms.[7][19] The standard method of diagnosis is by real-time reverse transcription polymerase chain reaction (rRT-PCR) from a nasopharyngeal swab.[22] Chest CT imaging may also be helpful for diagnosis in individuals where there is a high suspicion of infection based on symptoms and risk factors; however, guidelines do not recommend using CT imaging for routine screening.[23][24]
Recommended measures to prevent infection include frequent hand washing, maintaining physical distance from others (especially from those with symptoms), quarantine (especially for those with symptoms), covering coughs, and keeping unwashed hands away from the face.[8][25][26] In addition, the use of a face covering is recommended for those who suspect they have the virus and their caregivers.[27][28] Recommendations for face covering use by the general public vary, with some authorities recommending for them, some recommending against them (to conserve masks for healthcare workers), and others requiring their use.[28][29][30] There is limited evidence for or against the use of masks (medical or other) in healthy individuals in the wider community.[7]
According to the World Health Organization, there are no available vaccines nor specific antiviral treatments for COVID-19.[7] On 1 May 2020, the United States gave emergency use authorization to the antiviral remdesivir for people hospitalized with severe COVID‑19.[31] Management involves the treatment of symptoms, supportive care, isolation, and experimental measures.[32] The World Health Organization (WHO) declared the COVID‑19 outbreak a public health emergency of international concern (PHEIC)[33][34] on 30 January 2020 and a pandemic on 11 March 2020.[12] Local transmission of the disease has occurred in most countries across all six WHO regions.[35
Signs and symptoms
Fever is the most common symptom, although some older people and those with other health problems experience fever later in the disease.[5][36][unreliable medical source?] In one study, 44% of people had fever when they presented to the hospital, while 89% went on to develop fever at some point during their hospitalization.[5][37] A lack of fever does not verify someone is disease free.
Other common symptoms include cough, loss of appetite, fatigue, shortness of breath, sputum production, and muscle and joint pains.[1][5][6][38] Symptoms such as nausea, vomiting, and diarrhoea have been observed in varying percentages.[39][40][41] Less common symptoms include sneezing, runny nose, sore throat, and skin lesions.[42] Some cases in China initially presented with only chest tightness and palpitations.[43] A decreased sense of smell or disturbances in taste may occur.[44][45] Loss of smell was a presenting symptom in 30% of confirmed cases in South Korea.[13][46]
As is common with infections, there is a delay between the moment a person is first infected and the time he or she develops symptoms. This is called the incubation period. The average incubation period for COVID‑19 is five to six days but commonly ranges from one to 14 days,[7][47] with approximately 10% of cases exceeding that time.[48][49][50]
A minority of cases do not develop noticeable symptoms at any point in time
Complications
Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, septic shock, and death.[11][15][56][57] Cardiovascular complications may include heart failure, arrhythmias, heart inflammation, and blood clots.[58] Approximately 20-30% of people who present with COVID‑19 have elevated liver enzymes reflecting liver injury.[59][60] Neurologic manifestations include seizure, stroke, encephalitis, and Guillain–Barré syndrome (which includes loss of motor functions).[61] Following the infection, children may develop paediatric multisystem inflammatory syndrome, which has symptoms similar to Kawasaki disease, which can be fatal.[62][63]
Transmission
COVID‑19 is a new disease, and many of the details of its spread are still under investigation.[7][19][21] It spreads between people very efficiently and sustainably—easier than influenza but not as easily as measles.[19] This occurs mainly when people are in close contact (two metres or six feet) via small droplets produced during coughing, sneezing, or talking.[7][21] Contaminated droplets exhaled by infected people are then inhaled into the lungs, or settle on other people's faces to cause new infection.[19] The droplets are relatively heavy, usually fall to surfaces, and do not travel far through the air.[7][21] People can transmit the virus without showing symptoms, but according to the WHO and ECDC, it is unknown how often this happens.[7][19][21] One summary of available studies estimated the number of those infected who are asymptomatic to be 40%.[64]
People are most infectious when they show symptoms (even mild or non-specific symptoms), but may be infectious for up to two days before symptoms appear (pre-symptomatic transmission).[21] They remain infectious an estimated seven to twelve days in moderate cases and an average of two weeks in severe cases.[21]
When the contaminated droplets fall to floors or surfaces they can, though less commonly, remain infectious if people touch contaminated surfaces and then their eyes, nose or mouth with unwashed hands.[7] On surfaces the amount of active virus decreases over time until it can no longer cause infection,[21] and surfaces are thought not to be the main way the virus spreads.[19] It is unknown what amount of virus on surfaces is required to cause infection via this method, but it can be detected for up to four hours on copper, up to one day on cardboard, and up to three days on plastic (polypropylene) and stainless steel (AISI 304).[21][65][66] Surfaces are easily decontaminated with household disinfectants which kill the virus outside the human body or on the hands.[7] Disinfectants or bleach are not a treatment for COVID‑19, and cause health problems when not used properly, such as when used inside the human body.[67]
Sputum and saliva carry large amounts of virus.[7][19][21][68] Although COVID‑19 is not a sexually transmitted infection, kissing, intimate contact, and faecal-oral routes are suspected to transmit the virus.[69][70] Some medical procedures are aerosol-generating[71] and result in the virus being transmitted more easily than normal.[7][21]
Estimates of the number of people infected by one person with COVID-19 (the R0) have varied widely. The WHO's initial estimates of the R0 were 1.4-2.5 (average 1.95), however a more recent review found the basic R0 (without control measures) to be higher at 3.28 and the median R0 to be 2.79.[72]
Virology
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel severe acute respiratory syndrome coronavirus, first isolated from three people with pneumonia connected to the cluster of acute respiratory illness cases in Wuhan.[73] All features of the novel SARS-CoV-2 virus occur in related coronaviruses in nature.[74] Outside the human body, the virus is killed by household soap, which bursts its protective bubble.[23]
SARS-CoV-2 is closely related to the original SARS-CoV.[75] It is thought to have an animal (zoonotic) origin. Genetic analysis has revealed that the coronavirus genetically clusters with the genus Betacoronavirus, in subgenus Sarbecovirus (lineage B) together with two bat-derived strains. It is 96% identical at the whole genome level to other bat coronavirus samples (BatCov RaTG13).[42] In February 2020, Chinese researchers found that there is only one amino acid difference in the binding domain of the S protein between the coronaviruses from pangolins and those from humans; however, whole-genome comparison to date found that at most 92% of genetic material was shared between pangolin coronavirus and SARS-CoV-2, which is insufficient to prove pangolins to be the intermediate host.[76]
| Coronavirus disease 2019 (COVID-19) | |
|---|---|
| Other names | |
 | |
| Symptoms of COVID-19 | |
| Pronunciation | |
| Specialty | Infectious disease |
| Symptoms | Fever, cough, fatigue, shortness of breath, loss of smell; sometimes no symptoms at all[5][6][7] |
| Complications | Pneumonia, viral sepsis, acute respiratory distress syndrome, kidney failure, cytokine release syndrome |
| Usual onset | 2–14 days (typically 5) from infection |
| Causes | Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) |
| Risk factors | Travel, viral exposure |
| Diagnostic method | rRT-PCR testing, CT scan |
| Prevention | Hand washing, face coverings, quarantine, social distancing[8] |
| Treatment | Symptomatic and supportive |
| Frequency | 5,591,067[9] confirmed cases |
| Deaths | 350,458 (6.3% of confirmed cases) |

The WHO has published several testing protocols for the disease.[96] The standard method of testing is real-time reverse transcription polymerase chain reaction (rRT-PCR).[97] The test is typically done on respiratory samples obtained by a nasopharyngeal swab; however, a nasal swab or sputum sample may also be used.[22][98] Results are generally available within a few hours to two days.[99][100] Blood tests can be used, but these require two blood samples taken two weeks apart, and the results have little immediate value.[101] Chinese scientists were able to isolate a strain of the coronavirus and publish the genetic sequence so laboratories across the world could independently develop polymerase chain reaction (PCR) tests to detect infection by the virus.[11][102][103] As of 4 April 2020, antibody tests (which may detect active infections and whether a person had been infected in the past) were in development, but not yet widely used.[104][105][106] The Chinese experience with testing has shown the accuracy is only 60 to 70%.[107] The FDA in the United States approved the first point-of-care test on 21 March 2020 for use at the end of that month.[108]
Diagnostic guidelines released by Zhongnan Hospital of Wuhan University suggested methods for detecting infections based upon clinical features and epidemiological risk. These involved identifying people who had at least two of the following symptoms in addition to a history of travel to Wuhan or contact with other infected people: fever, imaging features of pneumonia, normal or reduced white blood cell count, or reduced lymphocyte count.[109]
A study asked hospitalised COVID‑19 patients to cough into a sterile container, thus producing a saliva sample, and detected the virus in eleven of twelve patients using RT-PCR. This technique has the potential of being quicker than a swab and involving less risk to health care workers (collection at home or in the car).[68]
Along with laboratory testing, chest CT scans may be helpful to diagnose COVID‑19 in individuals with a high clinical suspicion of infection but are not recommended for routine screening.[23][24] Bilateral multilobar ground-glass opacities with a peripheral, asymmetric, and posterior distribution are common in early infection.[23] Subpleural dominance, crazy paving (lobular septal thickening with variable alveolar filling), and consolidation may appear as the disease progresses.[23][110]
In late 2019, the WHO assigned emergency ICD-10 disease codes U07.1 for deaths from lab-confirmed SARS-CoV-2 infection and U07.2 for deaths from clinically or epidemiologically diagnosed COVID‑19 without lab-confirmed SARS-CoV-2 infection.[111]
Comments
Post a Comment